The four principles of family medicine
The family physician is a skilled clinician.
Family physicians demonstrate competence in the patient-centred clinical method; they integrate a sensitive, skillful, and appropriate search for disease. They demonstrate an understanding of patients’ experience of illness (particularly their ideas, feelings, and expectations) and of the impact of illness on patients’ lives. Family physicians use their understanding of human development and family and other social systems to develop a comprehensive approach to the management of disease and illness in patients and their families. Family physicians are also adept at working with patients to reach common ground on the definition of problems, goals of treatment, and roles of physician and patient in management. They are skilled at providing information to patients in a manner that respects their autonomy and empowers them to “take charge” of their own health care and make decisions in their best interests. Family physicians have an expert knowledge of the wide range of common problems of patients in the community, and of less common, but life threatening and treatable emergencies in patients in all age groups. Their approach to health care is based on the best scientific evidence available.
Family medicine is a community-based discipline.
Family practice is based in the community and is significantly influenced by community factors. As a member of the community, the family physician is able to respond to people’s changing needs, to adapt quickly to changing circumstances, and to mobilize appropriate resources to address patients’ needs. Clinical problems presenting to a community-based family physician are not pre-selected and are commonly encountered at an undifferentiated stage. Family physicians are skilled at dealing with ambiguity and uncertainty. They will see patients with chronic diseases, emotional problems, acute disorders (ranging from those that are minor and self-limiting to those that are life-threatening), and complex biopsychosocial problems. Finally, the family physician may provide palliative care to people with terminal diseases. The family physician may care for patients in the office, the hospital (including the emergency department), other health care facilities, or the home. Family physicians see themselves as part of a community network of health care providers and are skilled at collaborating as team members or team leaders. They use referral to specialists and community resources judiciously.
The family physician is a resource to a defined practice population.
The family physician views his or her practice as a “population at risk,” and organizes the practice to ensure that patients’ health is maintained whether or not they are visiting the office. Such organization requires the ability to evaluate new information and its relevance to the practice, knowledge and skills to assess the effectiveness of care provided by the practice, the appropriate use of medical records and/or other information systems, and the ability to plan and implement policies that will enhance patients’ health.
- Family physicians have effective strategies for self-directed, lifelong learning.
- Family physicians have the responsibility to advocate public policy that promotes their patients’ health.
- Family physicians accept their responsibility in the health care system for wise stewardship of scarce resources.
- They consider the needs of both the individual and the community.
The patient-physician relationship is central to the role of the family physician.
Family physicians have an understanding and appreciation of the human condition, especially the nature of suffering and patients’ response to sickness. They are aware of their strengths and limitations and recognize when their own personal issues interfere with effective care. Family physicians respect the privacy of the person. The patient-physician relationship has the qualities of a covenant – a promise, by physicians, to be faithful to their commitment to patients’ well-being, whether or not patients are able to follow through on their commitments. Family physicians are cognizant of the power imbalance between doctors and patients and the potential for abuse of this power. Family physicians provide continuing care to their patients. They use repeated contacts with patients to build on the patient-physician relationship and to promote the healing power of interactions. Over time, the relationship takes on special importance to patients, their families, and the physician. As a result, the family physician becomes an advocate for the patient.
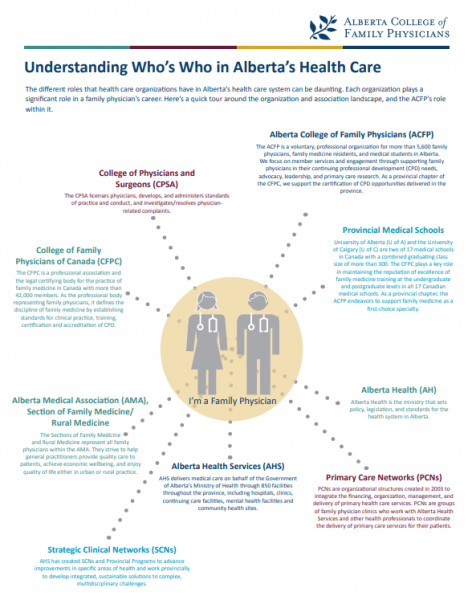
Learn More About Who’s Who in Alberta’s Health Care and ACFP’s Role Within It
CanMEDs-Family Medicine Competency Framework
CanMEDS-Family Medicine (CanMEDS-FM) is an adaptation of CanMEDS 2005, the competency framework for medical education developed by the Royal College of Physicians and Surgeons of Canada (RCPSC). It guides curriculum and forms the basis for the design and accreditation of residency programs.